
|
Halloween is only a few weeks away but there’s another season just around the corner that can be just as scary—the start of the flu season, which officially begins at the end of this month. In addition to causing kids to miss school and adults to call out sick from work, there is no denying that the flu can be deadly for thousands, and in some years, tens of thousands of Americans. The importance of getting a flu shot is something ECPs should advocate for themselves, their associates/staff and their patients as practice waiting rooms can be breeding grounds for spreading the flu.
According to the Centers for Disease Control (CDC), “Influenza is a potentially serious disease that can lead to hospitalization and sometimes even death. Every flu season is different, and influenza infection can affect people differently, but millions of people get the flu every year, hundreds of thousands of people are hospitalized and thousands or tens of thousands of people die from flu-related causes every year. An annual seasonal flu vaccine is the best way to help protect against flu. Vaccination has been shown to have many benefits including reducing the risk of flu illnesses, hospitalizations and even the risk of flu-related death in children.”
During the 2018-2019 flu season, the Centers for Disease Control and Prevention reported that about 45 percent of U.S. adults received the flu vaccine. While this is an increase of 8 percent from 2017-2018, it falls way below the national goal of 70 percent of American adults receiving a flu shot.
|
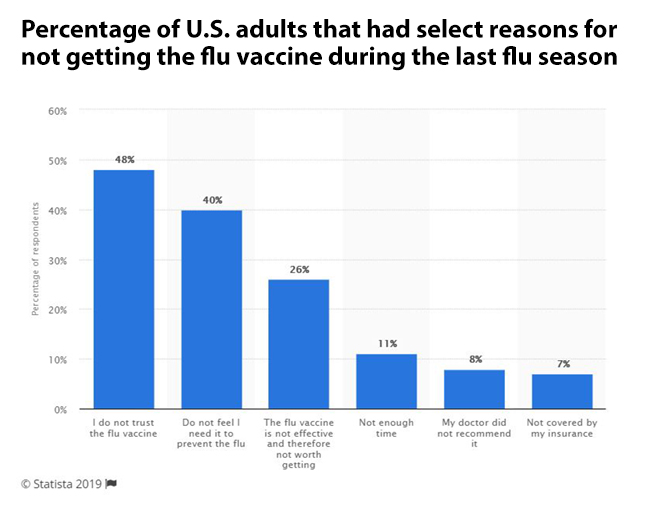
There are many reasons why people avoid getting the flu shot. This graphic from Statista.com depicts the percentage of U.S. adults that had select reasons for not getting the flu vaccine during the last flu season of 2018. According to the data, 48 percent of respondents did not get the flu vaccine because they did not trust the flu vaccine. And only 7 percent skipped the shot because they were not covered by their insurance.
The 2018-2019 influenza season was moderately severe, with activity beginning to increase in November, peaking in mid-February, and returning to below baseline in mid-April, the CDC said. However, the 21-week season was the longest in 10 years, according to the CDC's Morbidity and Morality Weekly Report.
The 2017-2018 flu was a much different story, however. That season, the percentage of deaths attributed to pneumonia and influenza was at or above the epidemic threshold for 16 consecutive weeks. The CDC estimated overall, there were 959,000 hospitalizations and 79,400 deaths during the 2017–2018 season.
The CDC was also able to specifically track the number of pediatric deaths due to the flu and the numbers indicate the 2017-2018 flu season was especially deadly for children. As of April 19, 2019, a total of 186 pediatric deaths had been reported to CDC during the 2017-2018 season. Approximately 80 percent of these deaths occurred in children who had not received a flu vaccination that season. Sadly, many of those pediatric deaths might have been avoided if the children, and those around them, had received the vaccine.
And what’s in store for this year’s flu season? Unfortunately there’s no definitive way to tell but there are some indicators out there which should make people sit up and take notice. Here’s what a recent New York Times feature had to say about this winter’s flu season.
“Australia had an unusually early and fairly severe flu season this year. Since that may foretell a serious outbreak on its way in the United States, public health experts now are urging Americans to get their flu shots as soon as possible. “It’s too early to tell for sure, because sometimes Australia is predictive and sometimes it’s not,” said Dr. Daniel B. Jernigan, director of the influenza division of the Centers for Disease Control and Prevention. “But the best move is to get the vaccine right now.” Australia’s current flu season was dominated by the H3N2 strain, as was the 2017 season in both countries. H3N2, which emerged for the first time in the 1968 “Hong Kong flu” pandemic, tends to cause more hospitalization and deaths than other strains. H3N2 may also dominate in the United States this year, Dr. Jernigan said, but it is too early to be sure. In some years, he said, different strains appear in various Southern Hemisphere countries, including New Zealand, Chile and South Africa.”
Older people, people with chronic health conditions and children are most vulnerable to the flu. Recently, a nurse’s Facebook post went viral after she urged everyone to get a flu shot this year. Here’s an excerpt from a WebMD feature describing her “powerful statement.”

|
“The flu shot is NOT always about you. It's about protecting those around you, who cannot always protect themselves.” Amanda Bitz writes that we shouldn’t just get vaccinated to keep ourselves healthy. Instead, it’s “for the grandparents, whose bodies are not what they used to be, and they just can't kick an illness in the butt like when they were young. For the 30-\ year old, with HIV or AIDS, who has a weakened immune system. For the 25-year-old mother of three who has cancer. She has absolutely zero immune system because of chemotherapy.”
Bitz goes on to build her case, citing heart-wrenching example after example, before concluding that everyone needs to do their part to keep others safe. “I have been in the room as a patient has passed away, because of influenza. I have watched patients struggle to breathe, because of influenza,” she writes. “Herd immunity is a thing. Influenza killing people is a thing. You getting the flu shot, should be a thing.”
Click here to read the full story from WebMD and click here to view a slideshow from WebMD titled “Do I Have the Flu?”
Editors Note: As I write this feature I am fighting off a cold, which is very bad timing since I am scheduled to get my flu shot next week, courtesy of my employer WebMD. If you are sick with a cold or the flu, it is recommended you do not get the flu vaccine. If you miss getting the flu shot at work or your employer doesn’t offer the flu vaccine, check with your medical insurer to see if you are covered to receive a flu shot at your local pharmacy.
The Facts and Myths About the Flu Vaccine
If you are on the fence about whether or not to get that flu shot this year, here are some facts and myths about the flu vaccine, courtesy of the Centers for Disease Control.
The Facts
Key reasons to get a flu vaccine
• Flu vaccine has been shown to reduce flu illnesses, hospitalization, and even death in children.
• Flu vaccination also is an important preventive tool for people with chronic health conditions.
• Vaccinating pregnant women helps protect them from flu illness and hospitalization, and also has been shown to help protect the baby from flu infection for several months after birth, before the baby can be vaccinated.
• While some people who get vaccinated still get sick, flu vaccination has been shown in several studies to reduce severity of illness.
The flu vaccine is safe
Flu vaccines have a good safety record. Hundreds of millions of Americans have safely received flu vaccines over the past 50 years. Extensive research supports the safety of seasonal flu vaccines. Each year, CDC works with the U.S. Food and Drug Administration (FDA) and other partners to ensure the highest safety standards for flu vaccines. More information about the safety of flu vaccines is available here.
Side effects from the flu shot
Flu shots are made using killed flu viruses (for inactivated vaccines), or without flu virus at all (for the recombinant vaccine). So, you cannot get flu from a flu shot. Some minor side effects that may occur include soreness, redness and/or swelling where the shot was given, low grade fever, and aches.
When and where to get vaccinated
You should get a flu vaccine by the end of October. However, as long as flu viruses are circulating, vaccination should continue throughout flu season, even in January or later. Flu vaccines are offered in many doctors’ offices and clinics. Flu vaccine is available in many other locations, including health departments, pharmacies, urgent care clinics, health centers, and travel clinics. Vaccines may also be offered at your school, college health center, or workplace.
The Myths
A flu vaccine gives you the flu
No, flu vaccines cannot cause flu illness. Flu vaccines given with a needle (i.e., flu shots) are currently made in two ways: the vaccine is made either with a) flu viruses that have been “inactivated” (killed) and that therefore are not infectious, or b) using only a single gene from a flu virus (as opposed to the full virus) in order to produce an immune response without causing infection.
It’s better to get the flu than the flu vaccine
No. Flu can be a serious disease, particularly among young children, older adults and people with certain chronic health conditions, such as asthma, heart disease or diabetes. Any flu infection can carry a risk of serious complications, hospitalization or death, even among otherwise healthy children and adults. Therefore, getting vaccinated is a safer choice than risking illness to obtain immune protection.
I don’t really need a flu vaccine every year
Yes, you do. CDC recommends a yearly flu vaccine for just about everyone 6 months and older, even when the viruses the vaccine protects against have not changed from the previous season. The reason for this is that a person’s immune protection from vaccination declines over time, so an annual vaccination is needed to get the “optimal” or best protection against the flu.
When I get a seasonal flu vaccine I still get sick with flu symptoms
There are several reasons why someone might get flu symptoms, even after they have been vaccinated against flu.
• One reason is that some people can become ill from other respiratory viruses besides flu such as rhinoviruses, which are associated with the common cold, cause symptoms similar to flu, and also spread and cause illness during the flu season. The flu vaccine only protects against influenza, not other illnesses.
• Another explanation is that it is possible to be exposed to influenza viruses, which cause the flu, shortly before getting vaccinated or during the two-week period after vaccination that it takes the body to develop immune protection. This exposure may result in a person becoming ill with flu before protection from the vaccine takes effect.
• A third reason why some people may experience flu like symptoms despite getting vaccinated is that they may have been exposed to a flu virus that is very different from the viruses the vaccine is designed to protect against. The ability of a flu vaccine to protect a person depends largely on the similarity or “match” between the viruses selected to make the vaccine and those spreading and causing illness. There are many different flu viruses that spread and cause illness among people. For more information, see Influenza (Flu) Viruses.
• The final explanation for experiencing flu symptoms after vaccination is that the flu vaccine can vary in how well it works and some people who get vaccinated may still get sick.

|